Fibrocystic changes (FCCs) (also called fibrocystic breasts, and formally called "Fibrocystic disease of the breast") define the presence or development of benign lumpy and/or ropey tissue in one or both breasts. These lumps or nodules result from an excess number of cells that grow in the breast. It is believed that the increase in cells is due to hormonal stimulation during the menstrual cycle due to a predominance of estrogen over PROGESTERONE.
Not uncommon, ~90% of American women have FCCs. Of these women, 40% are unaware they have them. FCCs generally affect premenopausal women aged 20-50.
Typical symptoms include:
Ultrasounds can be used to monitor changes to the breast. Solid-feeling lumps may be further investigated with a biopsy to rule out cancer.
FCCs are medically referred to as lesions, which are either proliferative (i.e. continuing to involve new cell growth) or non-proliferative. Non-proliferative lesions includes cysts, which are fluid /partially solid-filled round or ovoid nodules that can be moved around (since they are not attached to surrounding tissue). The proliferative lesions are solid and can not be moved, and some may have normal cells, while others may be comprised of some abnormal cells (referred to as atypia). It is the solid lesions which are the subject of debate as to whether their presence increases the risk for breast cancer. These are the lesion groups:
Most FCCs are benign and have no consequences. A large study of more than 9000 women over a 15 year period (Hartmann et al, 2005) determined that the risk of getting breast cancer after diagnosis of FCCs was:
• Inversely associated with the age at biopsy (i.e. younger women have a greater risk than older women). The risk was 6.99 times the expected risk among women who received a diagnosis of atypia before the age of 45 years; 5.02 times when diagnosed between 45 and 55 years and 3.37 times when it was diagnosed after 55 years of age. Women with nonproliferative lesions and no or weak family history had no increase in the risk of breast cancer.
Women with non-proliferative finding and a strong family history of BC. Risk of BC is 1.62 times expected rate. Another study found no difference (Dupont & Page, 1985)
Women with atypia (abnormal cells) with a family history of BC . Risk of BC is 4 times expected rate, regardless of the degree of family history.
Women with atypia (abnormal cells) without a family history of BC . Risk of BC is 2.95 times expected rate.
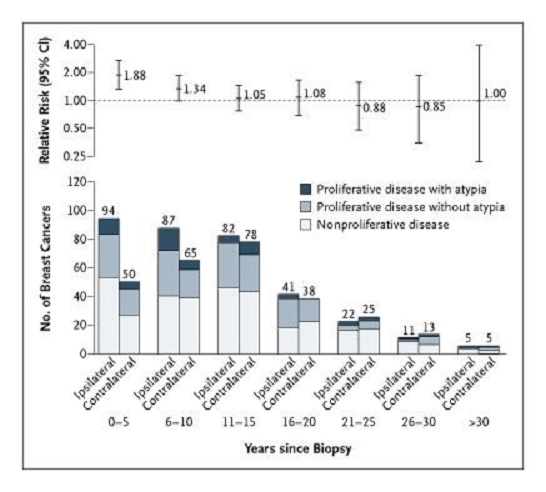
An excess of breast cancers occurred in the same breast with diagnosed FCCs during the first years of follow-up. Especially in women with atypia. (In the following chart, ipsilateral means BC occurred on same side, contralateral means on the other breast). The report suggests that the excess risk of cancer in the same breast in the first 10 years after diagnosed FCCs points to the presence of precursors for BC in some women. This author also questions whether the biopsy itself may have played a role in the excess BC numbers.
Over the last 80 years, hundreds of publications have confirmed statistical correlations between advanced fibrocystic breasts and subsequent breast cancer. i.e. The longer fibrocystic tissue is present in a breast, the higher the potential risk for developing breast cancer.
Accumulation of toxins in the breast may occur due to overuse of deodorants or from a tight-fitting bra which prevents proper lymph drainage from the breast
To keep the cell count steady in the breasts, some cells have to be removed each month. Leftover cells that have not been appropriately destroyed build up over repeated cycles and cause the lumpy, tender breasts, and larger fibrocystic lesions.
The breasts concentrate iodine when available. Several studies have demonstrated a relationship between low iodine intake and FCCs both in women and laboratory animals. A sufficiency of iodine eliminates the excess cells, enabling the breast to return to its normal resting state as the fibrocystic lumps slowly disappear from the breast.
Check out this lecture by Dr. David Brownstein about iodine and its deficiency relationship to breast cancer:
http://www.youtube.com/watch?v=tZJ9Bcqjgzc
If you discover you have FCCs at the age of 45-55, it is likely you have had it for many years, and there is a possibility that the cells may become cancerous. The good news is that it can be cleared up completely with a daily intake of iodine.
Derry, DM, Breast Cancer and iodine Preventing and surviving,Trafford Publishing company, Canada, 2001.
FCCs treated with Iodine Supplementation. In 1993 Ghent and Eskin published a landmark paper on the treatment of severe fibrocystic breasts with iodine supplements. This paper was the result of more than 30 years of research by Dr. Bernard. A. Eskin of the Medical College of Pennsylvania in Philadelphia. First in animals and then in humans, he proved fibrocystic breasts are the result of low dietary iodine. He has also shown that fibrocystic breasts can go on to develop into breast cancer. (Ghent et al, 1993; Eskin et al, 1995; Eskin, 1970; Eskin, 1983; Eskin, 1976; Eskin et al, 1986)
Pesticides, microbes, toxins, etc. If a person has enough iodine in the body, the toxins cannot do much damage because iodine does an excellent job of deactivating toxins.
Environmental estrogen look-alikes (xenoestrogens). It is likely that iodine helps eliminate FCCs (and ovarian cysts) at least partly through it's interaction with estrogens. Iodine helps the body to metabolize ESTRONE (a slightly carcinogenic human estrogen) and 16-alpha-hydroxyestrone (a much more dangerous metabolite of human estrogen) into ESTRIOL, an "anti-carcinogenic" or at the very least "neutral" form of human estrogen.
Prevention of FCCs. Based on their studies of iodine in women and female rats, Ghent et al and Eskin have estimated that the amount of iodine required for protection against breast cancer and fibrocystic breasts, is at least 20 to 40 times the amount required for control of goiter. Therefore, the MINIMUM amount of iodine required for control and prevention of fibrocystic breasts is equivalent to 0.1 mg/kg body weight/day (this is the amount used by Ghent et al).
E.g. the minimum daily amount of iodine for a 110# woman would be 5 mg.
With diagnosed FCCs. The pertinent question to ask is "What is the optimal amount of iodine that will restore and maintain normal breast function and histology, without any significant side effects and negative impact on thyroid functions?" (In Canada, 1975, Ghent et al tested various amounts of various forms of iodine in three open trials.5% Lugol's solution was used in 233 patients for 2 years in daily amounts ranging from 31 to 62 mg iodine, achieving clinical improvement in 70% of the patients. (Guy. E. Abraham M.D et al)
Unfortunately, if you have FCCs you don't know if they are precancerous lesions without a biopsy. On the other hand, fibrocystic breast lumps disappear by taking iodine in adequate daily amounts, so that you are essentially preventing breast cancer from occurring.
The best response for those with FCCs was observed with ingestion of about 50 mg iodine/iodide (E.g. 8 drops 5% Lugol's Solution or 4 Iodoral™) / day for several months (the same dose suggested for reversal of the cancerous phase).
How-to Supplement Iodine for whole body Sufficiency
Objective and subjective improvements of FCCs in response to various dosages of various forms of iodine or iodide. (Vishnyakova et al, 1966; Ghent et al, 1993; http://www.optimox.com/pics/Iodine/IOD-01/IOD_01.htm#42)
|
Study Design |
# pts |
Duration |
Form of I |
Daily Dosage |
% of pts. w/clinical improvement |
% of pts with side effects |
||
|
Open Trial |
200 |
3 years |
Potassium Iodide |
10-20 mg |
72% |
none reported |
||
|
Open Trial |
233 |
2 years |
Lugol 5%* |
5-10 drops (31-62 mgI) |
70% |
7% |
||
|
Open Trial |
588 |
5 years |
Iodine Caseinate |
10 mg |
40% |
9.5% |
||
|
Open Trial |
1365 |
18 months |
Aqueous Solution of Iodine |
0.08 mg/Kg BW |
74% |
10.9% |
||
|
Double Blind |
PL= 33 I2= 23 |
mean of 191 days |
Aqueous Solution of Iodine |
0.08 mg/Kg BW |
Object. PL = -3% I2 = 65% |
Subject. 33% 65% |
N / A |
|
PL = Placebo, Pts = Patients, BW=Body Weight
Dupont WD, Page DL. Risk factors for breast cancer in women with proliferative breast disease (1985). N Engl J Med;312:146-151. Link
Eskin BA et al (1995) Different tissue responses for iodine and iodide in rat thyroid and mammary glands, Biol Trace Element Res.
Eskin BA et al (1986) Etiology of mammary gland pathophysiology induced by iodine deficiency, Frontiers in thyroidology.
Eskin BA (1983) Iodine and breast cancer. Biol Trace Element Res
Eskin BA (1976 Dietary iodine and cancer risk. Lancet.
EskinBA (1970) Iodine metabolism and breast cancer. Trans NY Acad Sci.
Ghent WR et al (1993) Iodine replacement in fibrocystic disease of the breast. Can J Surg;
Guy. E. Abraham M.D et al "Optimum Levels of Iodine for Greatest Mental and Physical Health" Link
Hartmann, Lynn C et al, (July 2005) Benign Breast Disease and the Risk of Breast Cancer. N Engl J Med; 353:229-237 Link
(Vishnyakova et al, (1966) Vestn Akad Med Navk SSSR, 21:19-22.