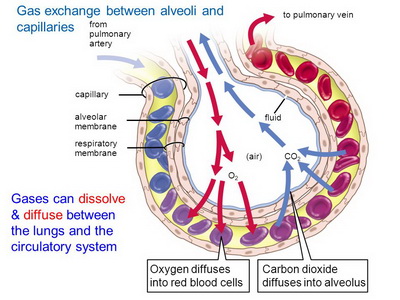
• Bring oxygen into the body and expel carbon dioxide. Oxygen travels through the wind pipe (trachea), bronchi and bronchioles to the alveoli (air sacs), where it diffuses through the thin alveoli walls and adjacent pulmonary capillaries (mini blood vessels) into the bloodstream; carbon dioxide travels the reverse pathway, diffusing from the bloodstream into the alveoli and out of the body via exhalation. This process requires the lung airways to expand and relax thousands of times a day.pathway, diffusing from the bloodstream into the alveoli and out of the body via exhalation. This process requires the lung airways to expand and relax thousands of times a day.
• Defend against infection by pathogenic airborne microbes and particulates:
• Hairs (cilia), twisted pathways, mucus-producing Goblet cells. Trap offenders
• Lysozymes in mucus / immune system macrophages. Trap and "eat" microbes, particulates, escorting them them out of the airways for swallowing
• Antioxidants defend against inhaled gases, particles and microbes. Chronic exposure to these offfenders can dramatically increase oxidation in the airways, with its resulting production of cell-damaging radicals. Lung-protective antioxidants of note include: ozone and nitrous oxide (both normally present in lung lining fluid}, glutathione (body's in-house water soluble antioxidant), Ascorbate (vitamin C), uric acid, resveratol (in red wine), and α-tochopherol (a form of vitamin E)
The M2 protein of the flu virus damages cells of the lung's inner lining, rendering them unable to remove fluid. This increases susceptibility to pneumonia and other lung diseases. Human airways transfected with virus type A protein, M2, increased damaging reactive oxygen species (ROS), but co-administration of an ester of the antioxidant glutathione prevented M2 from causing damage. M2 protein forms a tiny proton channel in the virion (complete infective form of virus outside host cell) essential for infection / viral replication.(M2 is the target of anti-influenza drugs: amantadine and rimantadine)
FIndings of Sadis Matalon and colleagues, Univ. of Alabama's Dept of Anesthesiology Pulmonary Injury and Repair Center.
• The trachea (windpipe) divides into 2 main bronchi, one for each lung
- The right primary bronchus. Divides into 3 secondary bronchi to supply the lungs 3 lobes
- The left primary bronchus. Divides into 2 secondary bronchi and then tertiary bronchi
• The bronchi branch off into smaller tubes called bronchioles like tree branches (airways branch an average of 23 times). Each of these eventually ends with a microscopic terminal bronchiole, which divides into the alveolar ducts, which end with alveoli (air sacs);
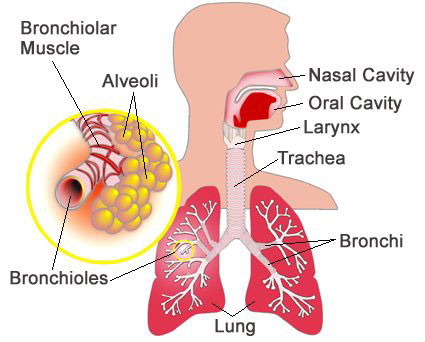
Pathway of Air: Nose => pharynx => larynx => trachea => primary bronchi => secondary bronchi => tertiary bronchi => bronchioles => terminal bronchioles => respiratory bronchioles => alveolar duct => alveoli
Mucus membranes line the inside of your respiratory tract i.e nose, mouth, windpipe, bronchi, bronchioles. Their purpose is to produce mucus (containing mucin) to lubricate the airways and to entrap any breathed in dust, particulates (e.g. carbon from smoking or long-term inhalation of city air), or disease-causing organisms (transporting them back to the pharynx for swallowing), and thus prevent them from accessing the lungs. If the membranes become inflamed they overproduce mucus, which may run down the nose or the back of the throat. Mucus is produced by submucosal/bronchial glands and goblet cells located between the epithelial lining cells. Mucus-producing glands undergoing prolonged exposure to irritants leads to their enlargement due to cellular replication.
The SMALLER bronchioles do not have cilia or mucus-producing cells, but they do have another type of secretory cell (called clara cells).
Muscle tone of bronchi / bronchioles. The diameter and length depends on smooth muscle tone of the these airways;
- Bronchi. Smooth muscle of bronchi contracts during expiration to expel air
- Bronchioles. If bronchiole muscles contract strongly, they can be almost completely shut (as can occur in an asthmatic attack);
Clean-up Crew - "Dust Cells"
A veritable "army" of alveolar macrophages, also called dust cells (macrophage means "Big eater" from Greek origin) reside in the lumen (inside) of alveoli and in the connective tissue between them, where they engulf and digest:
• Dust particles, particulates, and microbial "escapees" that managed to avoid the "mucus trap" higher up in the bronchotrachial tree
• Old blood cells from bleeding lungs
As many as 100 million macrophages each day carry their conquests out of the airways to be swallowed and digested.
The number of alveoli in an ADULT averages ~480 million. Aveoli have a total surface area of ~75 square meters [Pubmed]; their diameter is ~200µm (~2-3 times the width of an adult human hair), increasing during inhalation
Each alveolus is surrounded by blood capillaries. Supplied by small branches of the pulmonary artery
Type I - Wall structure cells
- Type I squamous alveolar cells form the main structure of the alveolar wall. They cover ~95% of alveoli surface
Type II - Repair and "non-stick" cells
- Comprise ~5% of alveoli surface. However, there are twice as many as structural wall cells; 80-90% phospholipids
- Can differentiate into poor substitutes for type 1 cells. Unable to replicate, and more susceptible to attack
- Two functions:
(1) Repair alveolar epithelium when squamous cells are damaged
(2) Secrete "non-stick" surfactant to coat inside wall of alveoli and smallest bronchioles. Prevents aveolus walls clinging together as alveolus deflates on exhalation, which would otherwise make it difficult for re-inflation on the next inhaled breath.
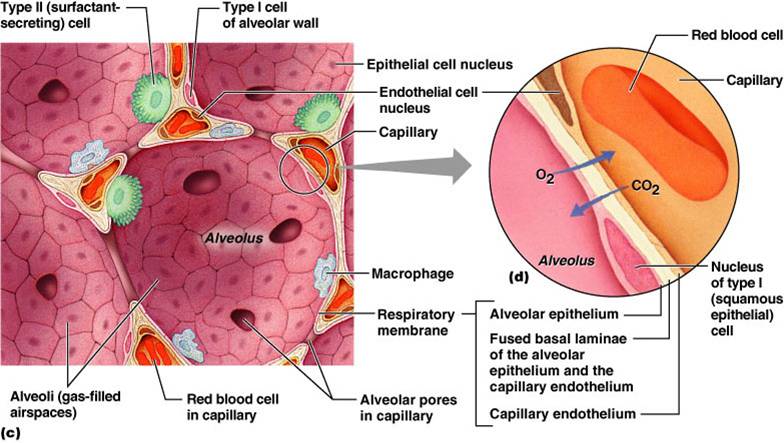
Respiratory membrane separates the alveolus from the pulmonary capillaries. This thin barrier (0.2-0.5µm) is comprised of the alveolar epithelial wall, a shared basement membrane and the capillary endothelium;