These include a family history of similar symptoms and a personal history of eczematous dermatitis, urticaria, and/or asthma.
The most blamed culprit is the allergen to which the I.S. is over-reacting. However, since some people are not affected by AR we should look to other explanations:
A study of nearly 4,300 German adults found that those whose partners had hay fever were at greater risk of developing such allergies themselves, and the longer couples lived together, the higher the hay fever risk climbed. The authors of the study published in the journal Allergy say the findings point to the importance of environment and lifestyle in the risk of developing allergies, since cohabitating couples have many of these factors in common.
An immune system that has a controlled, as opposed to overzealous response to allergens, requires:
- A balance of anti-inflammatory essential fats. In particular, there is a general excess of inflammatory omega-6 fatty acids typically found in grocery store oils and processed foods, and used in restaurants.
- An adequate supply of antioxidantsto combat reactive oxygen species (ROS) produced during the inflammatory process. Chronic inflammation can damage healthy tissue (called oxidative stress). Combative antioxidants would include:
• Vitamins A, B,C, E and flavonoids (E.g. quercetin). Found in fruits and vegetables and supplements;
• VITAMIN D. Produced in skin exposed to sunlight. VITAMIN D levels are lower in children who have allergies.
• MELATONIN. Hormone produced in the body during a good night's sleep
• Others. E.g. supplemental CoQ10.
• "In-house" antioxidants SOD, CAT, and GPx. Produced by body, but require antioxidant support nutrients including copper, iron, manganese, selenium and zinc.
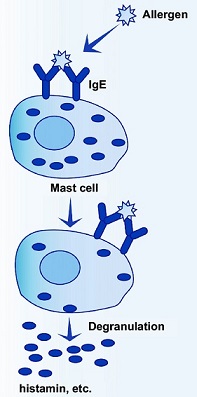
In most cases, AR is an allergic reaction to a specific allergen in the nasal mucosa. The allergen binds to the immunoglobulin E (IgE) antibody (specific to the allergen e.g. cat dander) on the surface of the immune system mast cell, which initiates:
- Initial-Response Phase -Recruitment of numerous chemoattractants and inflammatory mediators, which signal infiltration of eosinophils, basophils, neutrophils, and monocytes.
- Delayed-response phase (~2-8 hours after exposure)-inflammatory mediators in tissue lead to damage of mucosal epithelial cells. This phase is associated with increased sensitivity to allergens after repeated exposure and hyper-responsiveness to irritants.
Mast cells - are found in high concentrations in blood vessels of the sub-epithelial connective tissue of the respiratory tract and conjunctiva. Mast cell degranulation (release of active substances) accounts for ~ half AR symptoms.
HISTAMINE (main inflammatory mediator in AR) - is released by mast cells in the immediate-response phase and basophils in the delayed-response phase. When histamine binds to H1-receptors, it increases vasodilation, capillary permeability and smooth muscle contraction, resulting in rapid fluid leakage into nasal tissues and swollen, secretory nasal linings.
Evans R III. Epidemiology and natural history of asthma, allergic rhinitis, and atopic dermatitis. In: Middleton E Jr, Reed CE, Ellis EF, et al, eds. Allergy Principles and Practice 4th ed. St. Louis, MO: Mosby; 1993:1109-1136.