Ischemic Cardiovascular Disease (CVD)
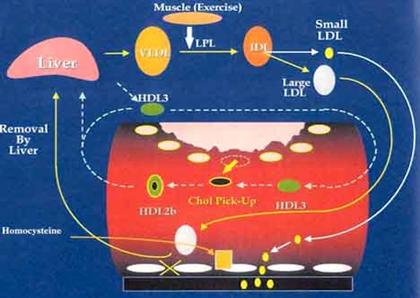
Since waxy cholesterol and fat are insoluble in water, they are transported in our "watery" blood and lymph inside spherical transporter capsules, called Lipoproteins. A single layer of phospholipids and "free" cholesterol encases the water-hating lipid core of triglycerides and cholesterol esters. Lipoproteins can carry, pick up or drop off cholesterol and fats.
Encircle lipoproteins to Regulate metabolism/uptake of lipoproteins
An apolipoprotein (a.k.a. apoprotein) is a coiled protein chain that drapes around a lipoprotein. Examples of apolipoproteins are Apo-A1, Apo-B100, and Apo (a)
- Keeps lipoproteins water-soluble for circulation in blood and lymph. Binds fat-soluble lipids to form water-soluble lipoproteins ;
- Helps maintain the structural integrity of the lipoprotein
- Can be a receptor ligand. As the "key" to open a receptor "lock" it can bind lipoproteins to cell surface receptors for interaction in tissues
• Apo-B100 and Apo-E bind to LDL-receptors. E.g. when a cell requires cholesterol, it synthesizes and inserts LDL receptors into its plasma membrane. LDL particles (lipoproteins) in the blood stream can then bind (via apolipoprotein) to these extracellular LDL receptors.
• Apo-AI bind to HDL receptors;
Apo(a) has binding sites (which act as "grappling hooks") that can bind to lysine or proline residues exposed in damaged arterial walls. Enables Lipoprotein (a) to orchestrate plaque formation for damage repair;
- Identifies the lipoprotein's type and determines from which cells cholesterol will be removed and to where it will be supplied
- Act as enzyme cofactors
- Examples of apolipoproteins include:
• Apo-AI - major protein content of HDL
• Apo-A4 - considered to be primarily involved in intestinal lipid absorption
• Apo-B100 - component of LDL and Lp(a) particles
• Apo-E - is a blood plasma protein; binds to a specific receptor on liver and peripheral cells; mediates LDL transport and uptake of cholesterol / lipids;
• Apo(a) -attached to Apo-B100 as a component of Lipoprotein (a)
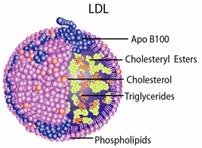
(Draped with a single Apo B100 apoprotein)
LDL (Low Density Lipoprotein) - this lipoprotein carries cholesterol TO tissues, including your arteries. It is sometimes labeled as "bad cholesterol", which is inappropriate since it is only doing the job of the fire-truck bringing the "water"(cholesterol) to the "fire"(damaged site) to deal with the problem;

(Mainly draped with Apo A1)
HDL - shuttles cholesterol AWAY FROM tissues, including your arteries, and hence why HDL is called "good cholesterol". HDL takes cholesterol back to your liver to be recycled, where it is put back into other lipoproteins for transport to tissues and cells that need it. Note that the body considers that cholesterol is "precious" enough to be conserved.
(The little "a" stands for adhesive)
.jpg)
Lp(a) is basically an LDL, with an attached "sticky" apolipoprotein, called Apo(a) - Like LDL cholesterol, Lp(a) contains an apolipoprotein called Apo B100, some phospholipids, and cholesterol itself, but in Lp(a), the Apo B100 is chemically (covalently) bonded to an additional large apolipoprotein known as Apo(a), which makes Lp(a) behave differently than LDL.
The presence of Apo(a) prevents Apo B100 of LDL binding to an LDL receptor
- Lp(a) carries substantial amounts of cholesterol - which can be readily extracted and accumulated at damage sites.
- Apo(a) is expressed by liver cells (hepatocytes) and the assembly of Apo(a) and LDL particles takes place in the liver
.gif)
- Lp(a) is a major independent risk factor for cardiovascular disease - in an attempt to patch lesions in the endothelial blood vessel wall and in response to an ascorbate deficiency, the liver manufactures cholesterol and its transporters Lp(a) and LDL. Both of these are "sticky", making them perfect for the job, although Lp(a) is much better in its patching ability.
"Sticky"Apo(a) has lysine and proline binding sites which it can use as "grappling hooks" to attach to lysine /proline residues
Attach either on:
(1) Molecules exposed in the extra cellular matrix (ECM) when arterial wall is damaged
- Lp(a) Binds to damaged arterial wall to form atherosclerotic plaques - Many U.S. National Medical Database reports confirm that "Sticky"Apo(a) targets the Lp(a) particle to damaged sites, adhering to amino acid (particularly lysine and proline) residues of collagen and elastin molecules, fibronectin, fibrinogen, GAGs, and proteoglycans exposed in the extracellular matrix (ECM)* of a damaged blood vessel wall (Adhesion is determined by the presence of calcium and magnesium ions).
*Proteoglycans are themajor components of ECM (the space between cells in an organism), they form large complexes to other proteoglycans, to hyalauran and to fibrous matrix proteins, such as collagen and elastin.
| Lp(a) has Lysine Binding Sites (LBS) (receptors) enabling it to bind to exposed lysine in damaged artery walls and make plaque |
|---|
|
Think of an LBS on an Lp(a) molecule as a simple lock, and only one "key"(lysine), will fit into the "lock"(LBS /receptor). There may be multiple receptors on an Lp(a) molecule, but once they are all filled up with "keys"(lysine), the Lp(a) molecule loses its ability to bind with any more "keys".When all the Lp(a) "locks"have "keys", Lp(a) will no longer be able to bind to the exposed lysine in the arterial wall to be able to create plaque. Lp(a) also has similar proline receptors. |
Or
(2) Fibrin (in a clot)
_binds_fibrin.jpg)
Lp(a) binds to fibrin
- Apo(a) prevents blood clot breakdown - blood coagulation is a complex event whereby platelets are trapped by fibrin (a thread-like protein) to form a plug to prevent bleeding.
• In normal hemostasis, a blood clot is eventually no longer required and is dissolved when lysine/proline residues on fibrin bind to lysine/proline binding sites on plasminogen - the precursor to the plasmin enzyme which dissolves the blood clot;
• However, being structurally similar to plasminogen, Apo(a) also has an affinity for lysine residues on fibrin and so inhibits the binding of plasminogen - preventing the formation of plasmin for breaking down blood clots.
| Blood Clotting Mechanisms |
|---|
 Two concurrent pathways produce THROMBIN, which coagulates blood. Thrombin converts soluble fibrinogen to insoluble fibrin and activates platelets, which aggregate to form a blood clot of platelets and red blood cells, enmeshed in a network of fibrin molecules over the wound site. Thrombin production is initiated by: (1) Tissue Factor (TF) expressed on the cell surface of the following TF-expressing cells in response to trauma (called extrinsic pathway): • Cells not normally exposed to flowing blood, when exposed by vessel damage. Such as sub-endothelial cells (e.g. smooth muscle cells) and cells surrounding blood vessels (e.g. fibroblasts). • WBC Monocytes, endothelial cells and platelets. TF expression is induced by inflammatory conditions (i.e. influenced by pro-inflammatory cytokines, such as IL-1α, IL-1β, and TNF-α) in response to trauma. Monocytes also express TF (and MMP-9) when induced by type I collagen, but expression is decreased by antioxidants Poitevin S et al, Type I collagen induces tissue factor expression and MMP-9 production in human primary monocytes through a redox-sensitive pathway, 2008; (2) Blood contact with exposed molecules in damaged sub-endothelial surface (called intrinsic pathway). Blood contact activation pathway produces thrombin without requiring TF. Amplifies first pathway. |
The size of the cholesterol-carrying lipoprotein particle determines if it can fit through the gap between the endothelial cells lining the artery - which is about 26nm(1 nanometer = 10 -9 meter).
- LDL particles are in the range from 20-30 nm, those < 25.8 nM can get through easily - those > 26.3 nm can not. The presence of small LDL particles is associated with the degree of atherosclerosis.
- HDL particles ranging from 5-10 nm easily pass through the endothelial cell gaps