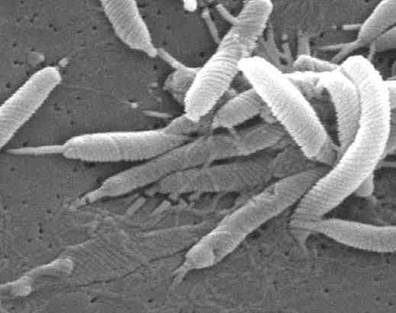
H. pylori is a common bacteria infecting about half of world'spopulation, with higher prevalence in developing countries.
The bacteria H. Pylori are responsible for ~75% of all gastric ulcers. In these cases, ulcers are a consequence of their burrowing into the stomach lining and causing inflammatory damage. H. Pylori presence is normally controlled by a sufficient acidity level in the stomach. . H. pylori can survive in the harsh acidic environment of the stomach because they produce the urease enzyme that promotes ammonia production around them to neutralize stomach acid. However, this study found that their glucose metabolism was irreversibly inhibited at the normal healthy stomach acid pH of <3.5.
Nobel Prize recipient Marshall induced gastritis in himself by consuming H. Pylori. He was then able to treat the gastritis using a 14 day dual therapy with bismuth salts and metronidazole. Marshall and Warren went on to show that antibiotics are effective in the treatment of many cases of gastritis. In 1994, the Nation Institutes of Health (USA) published an opinion stating that most recurrent gastric ulcers were caused by H. pylori, and recommended that antibiotics be included in the treatment regimen. Wikipedia
Bacteria usually enters the body via food and drink, but may also be contacted through mouth-to-mouth contact such as kissing. Researchers have found H. pylori in the saliva of some infected people.
Rapid urease test (RUT) (Also called campylobacter-like organism (CLO) test). Used to diagnose the presence of H. Pylori in a biopsy sample taken from stomach's gastric mucosa at ulcer site during gastroscopy.
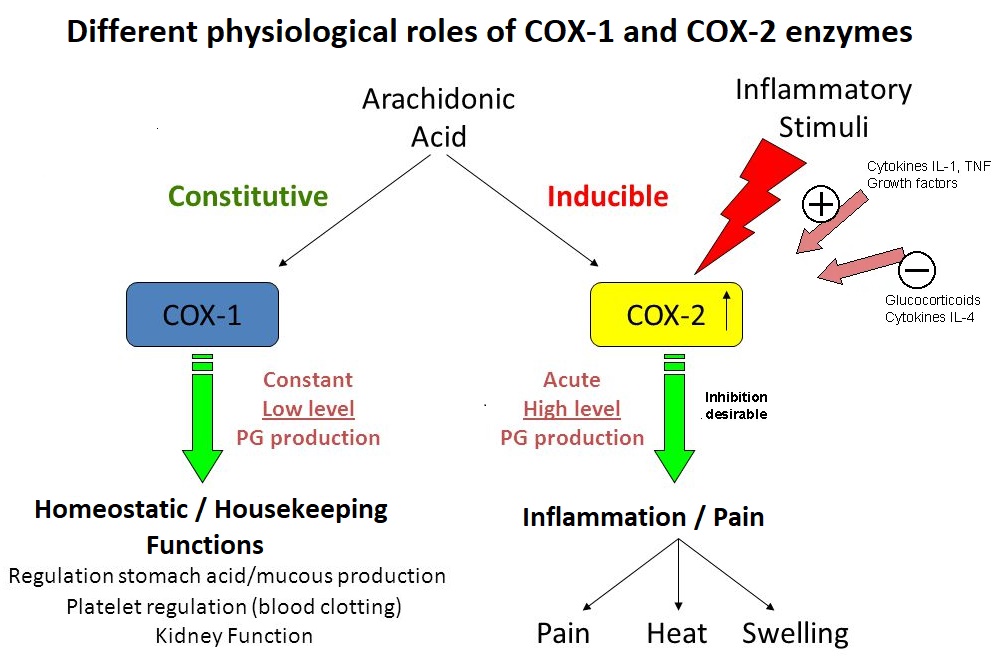
Cox-1 inhibiting NSAIDS (Non-steroidal anti-inflammatory drugs)
Regular, excessive or prolonged use of traditional (COX-2 and COX-1 enzyme inhibiting) NSAIDs is a well recognized cause of peptic ulcers and gastritis (inflammation of the stomach lining). Traditional NSAIDS include aspirin (Beyer®), ibuprofen (Motrin®, Advil®), naproxen (Aleve®) ; The more recent selective COX-2 enzyme inhibitors include Celebrex® and the infamous rafecoxib (Vioxx®, recalled in 2004 after being responsible for an estimated 60,000 deaths due to heart problems). Traditional NSAIDs (Not COX-2 selective) inhibit the COX-1 enzyme in the GI tract, reducing prostanoid synthesis from arichidonic acids (AAs). In particular, reducing prostacyclin (PGI2) and prostaglandin PGE2 with their protective effects for the stomach lining mucosal cells (gastric mucosa) can lead to erosion, ulceration, perforation and hemorrhage.
Prostaglandins prostacyclin (PGI2) and PGE2 are crucial to reducing acid secretion by gastric mucosa's parietal cells Dini, 2017, and maintaining healthy gastric mucosa by increasing blood flow to damage site and increasing mucus secretion to better protect lining from stomach acid.
COX-1 inhibiting NSAIDs reduce prostaglandins PGI2 (prostacylin), PGD2, PGE2 PGF2α-, and thromboxane TXA2.
Chart of Specific Eicosonoid (including prostaglandins) Effects
• Risk increases in women and anyone older than 60. Some NSAIDS are stronger COX-1 inhibitors than others.
A malignant tumor causes about 4% of gastric ulcers
• Stress
• Excess alcohol consumption. Alcohol has the potential to harm the stomach lining by stimulating gastric juice production (intended to digest protein molecules), even when food is not present.
• Family history of ulcers
• Smoking
• Use of corticosteroids.
• Improper diet, irregular or skipped meals. Dietary factors causing stomach ulcers in pigs (mammals with one stomach, like us) are:
Low protein / Low fiber diets.
Levels of wheat in excess of 55%.
Deficiencies of vitamin E or selenium.
Diets containing high levels of iron, copper or calcium and/or low in zinc.
Diets with high levels of POLYUNSATURATED fats.
Diets based on skimmed milk.
Footnote: pig ulcers occur at the top of the stomach and human ulcers toward the bottom.
• Chronic disorders such as liver disease, emphysema, rheumatoid arthritis may increase vulnerability to ulcers
Note: Spicy food CANNOT CAUSE stomach ulcers, but can aggravate an existing stomach ulcer.
• The elderly and women;
• Having rheumatoid arthritis, severe systemic disease or previous history of gastroduodenal bleeding;
• Using anti-thrombotic medication, corticosteroids, or high doses of NSAIDs;
Drini M. (2017). Peptic ulcer disease and non-steroidal anti-inflammatory drugs. Australian prescriber, 40(3), 91-93. doi:10.18773/austprescr.2017.037 Link