Dental plaque, dental caries and periodontal disease in humans result from actions initiated by normal bacterial flora as they have developed a costly symbiosis with humans
Dental Plaque is bacteria-laden material adhering to the teeth - which consists of:
• Bacterial cells (60-70% the volume of the plaque)
• Salivary polymers
• Bacterial extracellular products.
- Plaque is a naturally-constructed biofilm, with bacteria reaching a thickness of up to 300-500 cells on the surfaces of the teeth. Such accumulations subject the teeth and gingival tissues to high concentrations of bacterial metabolites, which result in dental disease.
- With no contest, the dominant bacterial species responsible for dental plaque are Streptococcus sanguis and Streptococcus mutans
- Plaque formation is initiated by weak attachment of streptococcal cells to salivary glycoproteins. Forming a thin film (pellicle) on the surface of the teeth. Next, a stronger attachment is formed by extracellular sticky polymers of glucose (glucans) synthesized by the bacteria from dietary sugars (mainly sucrose).
- Attachment of S. mutans and the formation of glucans is mediated by glycosyl transferase. This enzyme located on the cell surface of Streptococcus mutans is involved in both initial attachment of the bacterial cells to the tooth surface and in the conversion of sucrose to dextran and levan polymers (glucans) which form the extracellular matrix of plaque. Attachment can be prevented by the specific antibody to the enzyme.
Dental Caries is the destruction of the enamel, dentin or cementum of teeth due to bacterial activities
- Caries are initiated by direct demineralization of the enamel of teeth due to lactic acid and other organic acids which accumulate in dental plaque - Lactic acid bacteria in plaque produce lactic acid by fermenting the host's dietary sugars and other carbohydrates.
- Streptococcus mutansis considered the most likely culprit associated with the initiation of dental caries - but other lactic acid bacteria are probably involved as well. These organisms normally colonize the occlusal fissures (see diagram) and contact points between the teeth, correlating with decay on these surfaces.
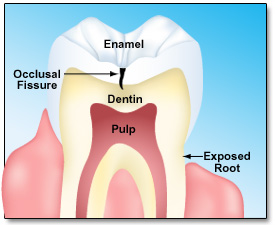
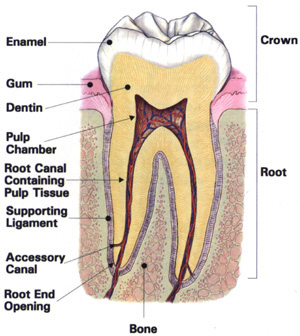
Cross section of a tooth illustrating the various structural regions susceptible to colonization or attack by microbes
Periodontal Diseases are bacterial infections affecting teeth support structures (gingiva, cementum, periodontal membrane and alveolar bone).
- Gingivitis is an inflammatory condition of the gums - associated with bacterial plaque build-up in the affected area. Increased presence of ACTINOMYCES are suggested as the cause. Diseases confined to the gum do not usually lead to loss of teeth.
- More serious forms of periodontal disease affect periodontal membrane and alveolar bone - and can result in tooth loss. Bacteria in these lesions are consist of GRAM-POSITIVE organisms (including ACTINOMYCES and streptococcI) and Gram-negative organisms (including spirochetes and Bacteroides). The mechanisms of tissue destruction in periodontal disease are not clearly defined but hydrolytic enzymes, endotoxins, and other toxic bacterial metabolites seem to be involved.
|
BACTERIUM |
Plaque |
Dental caries |
Gingivitis |
Periodontitis |
|
Streptococcus sanguis |
++ |
++ |
++ |
+ |
|
S. mutans |
++ |
++ |
0 |
0 |
|
S. salivarius |
0 |
0 |
0 |
0 |
|
ACTINOMYCES VISCOSIS |
+ |
+ |
++ |
+ |
|
A. ISRAELI |
+ |
+ |
++ |
++ |
|
LACTOBACILLUS sp. |
+ |
+ |
0 |
0 |
|
PROPIONIBACTERIUM ACNES |
0 |
+ |
+ |
++ |
|
Bacteroides sp. |
0 |
0 |
+ |
++ |
|
Selenomonas sputagena |
0 |
0 |
+ |
++ |
|
Large spirochetes |
0 |
0 |
0 |
++ |
++ = Frequently encountered in high proportions;
+ = Frequently encountered in low to moderate proportions;
0 = Sometimes encountered in low proportions or not detectable.
Modified from Davis, et al.: Microbiology. 4th ed. J. B. Lippincott. Philadelphia, 1990.
Kenneth Todar, PhD. Online Textbook of BacteriologyIn the GI Tract