ESTRIOL is one of the 3 main estrogen hormones - the other two are ESTRADIOL and ESTRONE.
ESTRIOL prevents menopausal symptoms. E.g. hot flashes, without causing unwanted side effects common to conventional estrogen replacement therapy.
- Vaginal dryness, atrophy (leading to vaginitis and cystitis). Beneficial acid-producing vaginal Lactobacilli depend on the presence of estrogen. ESTRIOL has a binding affinity to vaginal ERs equal to ESTRADIOL, sufficient to exert a full effect on the vagina after a single dose. For postmenopausal vaginal dryness and atrophy, which can lead to vaginitis and cystitis, ESTRIOL supplementation is theoretically the most effective and safest estrogen choice.
Study shows ESTRIOL modifies the vaginal flora and significantly lowers vaginal pH (from 5.5 to 3.8).
- ESTRIOL recolonized Lactobacilli (absent prior to therapy) in the vagina after only one month. In 61% of postmenopausal women given ESTRIOL, but in none receiving placebo.
- Additionally, the prevalence of Enterobacteriaceae (fecal bacteria) colonization fell from 67% to 31%. No change observed in those receiving placebo. (Cardozo et al,1998)
ESTRIOL may offer cancer-protective benefits for post menopausal women without the side effects of ESTRADIOL
ESTRIOL's WEAKNESS IS ITS STRENGTH.
ESTRIOL has a much less stimulating effect on the breast than ESTRONE and ESTRADIOL (which is 1000 times more stimulating to breast tissue)
ESTRIOL blocks ESTRONE and ESTRADIOL activity. ESTRIOL binds to estrogen receptors (ERs) on the breast cells, but has much weaker activity. Thus, it actually blocks the stronger ESTRONE and ESTRADIOL from binding to those cells and subjecting them to the subsequent higher estrogenic activity.
ESTRIOL ▲ correlates with cancer▼. In the 1966 Journal of the American Medical Association H.M. Lemmon, M.D. reported a study showing that higher levels of ESTRIOL in the body correlate with remission of breast cancer. Dr. Lemmon demonstrated that women with breast cancer had reduced urinary ESTRIOL excretion. He also observed that women without breast cancer have naturally higher ESTRIOL levels, compared to ESTRONE and ESTRADIOL levels, than women with breast cancer.
ESTRIOL has a much less stimulating effect on uterine lining than ESTRADIOL
Estrogens are needed for producing the proteins collagen and elastin. These give skin its elasticity and structure, and also hyaluronic acid, responsible for holding moisture in the skin.
- Collagen is lost at a rate of ~30% in first 5 years after menopause. Then ~ 2.1%/year over 20 years.
- You need a "Goldilocks" Dose" of ESTRIOL. i.e. it must be just right, because estrogen levels too high or too low give lower collagen levels.
Estrogen replacement therapy significantly increases dermal skin thickness. Determined by various studies.
Estriol is available as an oral supplement. However, via this route, the ESTRIOL must navigate through the digestive system and the liver will "dump" approximately 75% of the estriol into the body's elimination channels. A typical 2-5mg dose will thus yield only about 0.5mg. of ESTRIOL whilst also burdening the liver.
Estriol is better delivered topically or intravaginally using an estriol cream. The skin does not absorb ESTRIOL quite as well as ESTRADIOL or ESTRONE, but studies have shown that topical delivery is about 20 times more efficient than oral delivery. The skin and vaginal membranes also provide quite a steady supply of ESTRIOL until it clears the body - usually in 2 days.
It would make sense to apply cream in the area where it is needed. If in the reproductive area, then rubbed inside the vagina or into the testicle skin. Alternatively, if using it to treat facial wrinkles, then apply to the face and neck.
Estrogen receptors have been identified in the vulva, vagina, bladder, urethra, pelvic floor musculature, and endopelvic fascia. ESTRIOLhas a binding affinity to vaginal ERs equal to ESTRADIOL. Number of ERs varies by location:
ER and PR concentration remains stable postmenopause. However, AR (androgen receptor) concentration decreases by about half ;
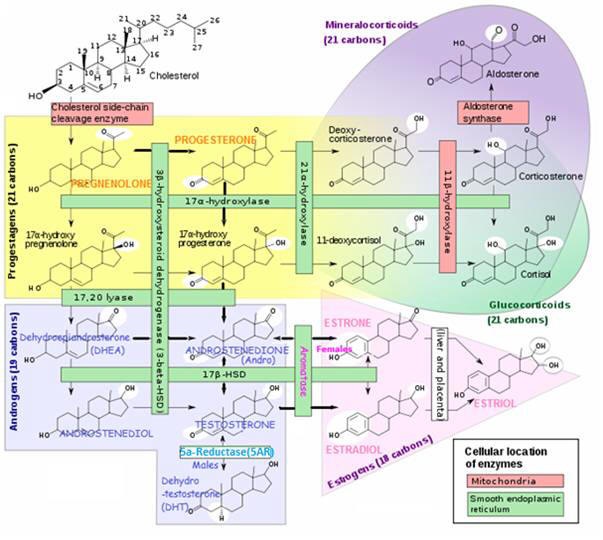
PROGESTERONE. To prevent hormone imbalance, any supplemental estrogen should be used together with Natural PROGESTERONE . According to Dr. Lee, most women become deficient in PROGESTERONE long before estrogen levels drop to the point of causing symptoms.
Vitamin E. Administered at 400 IU / day with ESTRIOL therapy will improve ESTRIOL activity and effectiveness
Use 0.5 mg - 0.75 mg topical or intravaginal ESTRIOL cream every other day or just a few times a week (responding to amount needed to control symptoms) See ESTRIOL Health Benefits for doses used in studies for specific problems.
Take a break from using ESTRIOL at the same time you take a break from PROGESTERONE. E.g. If you are postmenopausal or have had a hysterectomy, you use PROGESTERONE for only 3 weeks out of the month
Potency of ESTRADIOL is not much different to ESTRONE and ESTRIOL WHEN THEY ARE CONTINUOUSLY SUPPLIED (E.g. by implants or a patch) - Earlier work from the Clark laboratory maintained that physiological Estrogens, other than ESTRADIOL, were not weak when their concentrations were maintained continuously by implants (as opposed to single injections), in which case, they could actually elicit tissue growth of the uterus. Anderson JN etal, 1975
Also, continuous administration of ESTRIOL was shown to induce breast tumors in rodents, whereas a single injection failed to induce tumors in susceptible rodent strains and appeared to block such induction by ESTRADIOL and ESTRONE.
In the 1940's, Alexander Lipshuts demonstrated that a CONTINUOUS, WEAK estrogenic stimulus was immensely effective in producing first fibromas, then cancer, in one organ after another. The effect was not limited to the reproductive system. For example, the brain and liver, which also have estrogen receptors, may grow tumors too. Townsend Letters, 1997
ESTRIOL has been suggested as having a protective role in breast cancer based on the observation that oriental women who have a high ESTRIOL / (ESTRADIOL + ESTRONE) ratio in their blood also have a low incidence of breast cancer.
Anderson, J. N., Peck, E. J., Jr., and Clark, J. H. (1975) estrogen-induced uterine responses and growth: relationship to receptor estrogen binding by uterine nuclei. Endocrinology 96, 160-167
Cardozo L, Bachmann G, McClish D, Fonda D, Birgerson L. (1998) Meta-analysis of estrogen therapy in the management of urogenital atrophy in postmenopausal women: second report of the hormone and urogenital therapy committee. Obstet Gynecol ;92:722-7.
Dessole S, Rubattu G, Ambrosini G et al (2004 Jan) Efficacy of low-dose intravaginal estriol on urogenital aging in postmenopausal women. Menopause. ;11(1):49-56.
Minaguchi H, Uemura T, Shirasu K, et al (1996 Jun) Effect of estriol on bone loss in postmenopausal Japanese women: a multicenter prospective open study. J Obstet Gynaecol Res.;22(3):259-65.
Nishibe A, Morimoto S, Hirota K, et al (1996 May) Effect of estriol and bone mineral density of lumbar vertebrae in elderly and postmenopausal women. Nippon Ronen Igakkai Zasshi. 33(5):353-9.
Raz R, Stamm WE (1993) A controlled trial of intravaginal estriol in postmenopausal women with recurrent urinary tract infections.N Engl J Med ;329:753-7.
Takahashi K, Okada M, Ozaki T, et al (2000 May) Safety and efficacy of oestriol for symptoms of natural or surgically induced menopause. Hum Reprod.; 15(5):1028-36.
Townsend Letters for Doctors and Patients (January, 1997 issue), Ray Peat, a renowned biologist in the U.S.